These days, women have many different options when it comes to birth control. Forms of hormonal birth control are not only convenient but are also the most effective. In fact, when used properly hormonal birth control is 99.9% effective[1]. That being said, there is some discussion about hormonal birth control increasing breast cancer risk – but is this true? Hearing that hormonal birth control methods can increase the risk of breast cancer can be frightening due to the widespread use of contraceptives. Many women are concerned about this risk and wonder what their options are.
There are several kinds of hormonal contraceptives available. The differences between them include the type of hormone or combination of hormones in the contraceptive, the level of hormone, and the way in which the hormone is absorbed by your body.
Hormonal birth control preparations may contain estrogen or progesterone or a combination of the two. Different types of hormonal birth control include:
Oral birth control pills
This type of birth control contains two hormones; estrogen and progestin, which is a form of progesterone. When you take the combination pill, it prevents the eggs in your ovaries from maturing so you will not ovulate. You will not become pregnant because there is no egg to be fertilized by a sperm. Typically, the combination pill comes in a 21-pill pack or a 28-day pack. You take the pills for 21 consecutive days then no pills for the subsequent seven days, or you take active pills for 21 days and then placebo pills for the next seven days. The placebo pills are designed to help you remember to take your pill every day. Recently, new oral birth control pills have been developed, which enable you to take combination pills continuously for several months at a time. These methods reduce the number of periods you experience.
Another oral option is the mini pill, which contains only progestin. This hormone thickens the mucus lining of the cervix, making it difficult for sperm to pass through. It also reduces the chance of a fertilized egg implanting in the uterus. This option is usually recommended for women who must not take estrogen hormones for medical reasons.
Hormone implants
Birth control implants are inserted beneath the skin in your upper arm. The implant consists of a matchstick-sized rod. It prevents pregnancy by releasing the progestin, which thickens cervical mucus to make it difficult for a sperm to reach your egg. It also prevents ovulation. An implant can last for up to four years.
Birth control injections
The birth control injection is comprised of depot medroxyprogesterone acetate (DMPA), which is a long-acting, synthetic form of progesterone. This form of birth control contains no estrogen. Like the other progesterone-based methods, it thickens the cervical mucus and restricts the sperm’s access to the egg and preventing the release of an egg from the ovaries. The DMPA injection is administered by your doctor every 12 weeks. It must be administered within the first five days of your period. Once you have received the injection, you are protected within 24 hours. Your periods may stop altogether after you have been using DMPA for twelve months. This happens because the hormones cause the ovaries to go into a resting state. Your regular menstrual cycle should resume within 6 to 18 months after you have stopped taking the injections.
Birth control patches
Adhesive hormonal birth control patches deliver birth control through the skin. The patch, which is about the size of a quarter, can be worn on your arm, buttocks or abdomen. It must make good contact with the skin; this may be a problem if you swim, perspire heavily or take frequent showers, as moisture can make the patch less effective. You will wear each patch for a week then replace it with a new one. Like the combination pill, these patches contain both estrogen and progesterone. Also, like the pill, the patch suppresses ovulation.
Vaginal rings
This is a ring-shaped device which is placed inside the vagina. It contains estradiol and etonogestrel, which is a form of progestin. You will keep the vaginal ring in place for three weeks after which time you will remove it for one week to enable your period. The ring releases low levels of the hormones continuously for three weeks. The hormones are absorbed into your bloodstream and prevent pregnancy by stopping your ovaries from releasing eggs. They also cause thickening of cervical mucus, preventing sperm from reaching and fertilizing an egg.
Hormonal Intrauterine Device (IUD)
A hormonal IUD is a plastic, T-shaped device which is implanted in your uterus. The device continuously releases very small amounts of progestin into your body and can remain in place for up to six years. Like many other hormonal birth control methods, this type of IUD prevents pregnancy by thickening cervical mucus, so sperm cannot make it to an egg. It also stops your ovaries from releasing eggs.
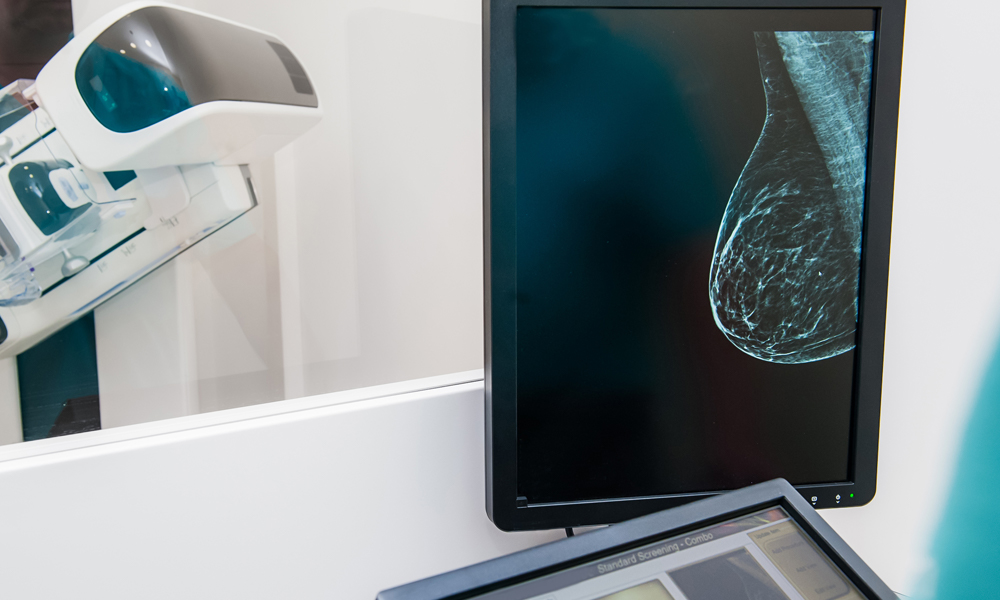
Does Hormonal Birth Control Increase the Risk of Cancer?
A 2017 study, published in the New England Journal of Medicine, showed that although this type of birth control increases the risk of breast cancer, the risk is very small[2].
A total of 1.8 million Danish women participated in the study. To qualify they had to be between the ages of 15 and 49. Each had no form of cancer at the time of the study or prior, and no history of blood clots. The researchers studied the women’s health for around ten years. During the course of the study, 11,517 cases of breast cancer were reported among the participating women.
The study showed a slightly elevated risk of breast cancer among users of contraceptive patches, hormonal birth control pills, vaginal rings, and also progestin-only implants such as injections, implants, and hormonal IUDs.
Though the research findings are credible, it’s important to remember that the study was observational, so there is a possibility that other factors that were not measured, may have led to the association between hormonal birth control and breast cancer.
There have been numerous studies on hormonal birth control methods and the risk of cancer over the past several decades. According to medical experts, the risk is much lower these days than it was during the 1980’s because modern hormonal birth control options contain smaller amounts of hormones than they did back then.
If you stopped using hormonal birth control some years ago, your risk of breast cancer is about the same as that of women who have never used hormonal birth control. However, if you are over 40 and you have a high risk of developing breast cancer, you should talk to your physician about switching to a non-hormonal option.
Does Hormonal Birth Control Have Protective Benefits?
Despite the slightly elevated risk of breast cancer in women who choose hormonal birth control, it can also have benefits other than preventing pregnancy. It can improve acne, reduce heavy and painful periods, ease symptoms of PCOS, and reduce symptoms of endometriosis. Furthermore, according to a 2013 review published in Obstetrics and Gynecology, women who take hormonal birth control pills are less likely to develop ovarian cancer. The risk decreases the longer you take this form of birth control and the benefits can continue for up to 30 years after you have stopped taking them.
If you are using or considering using hormonal birth control, whichever method you choose should be based on multiple factors. These include your health, age, and whichever method you find most comfortable. Overall, it would seem that the benefits of hormonal birth control outweigh the slight risk. But if you are concerned about the risk of breast cancer, talk to your physician about your options so that you can make an informed decision.
Have you switched your type of birth control to lower your breast cancer risk? Leave us a comment below and let us know – we would love to hear from you. Learn more about anti-estrogen foods, the truth behind soy and all about menopause in these other popular articles about hormones.